Autoimmune-induced seizures in adults with no history
Seizures in adults with no seizure history can be caused by a number of factors ranging from high blood pressure, drug abuse and toxic exposures to brain injury, brain infection (encephalitis) and heart disease. Mounting evidence also indicates that an immune dysfunction or abnormal autoimmune activity can elicit a sudden onset of seizures in adults with no history of the illness. 2
Seizures in adults with no seizure history can be caused by a number of factors ranging from high blood pressure, drug abuse and toxic exposures to brain injury, brain infection (encephalitis) and heart disease.
Immune dysfunction or abnormal autoimmune activity can elicit a sudden onset of seizures in adults with no history of the illness. 2
It’s well-established that people with certain autoimmune disorders, such as lupus, type 1 diabetes, celiac disease, multiple sclerosis, rheumatoid arthritis, and psoriasis, are at greater risk of developing epileptic seizures. Studies put the risk as high as 4-fold in adults and 5-fold in children.³ According to researchers, “Immune dysfunction may be partly responsible for this association.” 4
Investigators from Mayo Clinic point out, “It’s now a recognized and accepted fact that a proportion of patients with new-onset epilepsy can have an autoimmune etiology.” 5 Individuals with autoimmune-induced seizures typically do not respond to traditional seizure medications and treatments, and are often classified as having drug resistant epilepsy. 5
“It’s now a recognized and accepted fact that a proportion of patients with new-onset epilepsy can have an autoimmune etiology,” according to investigators from Mayo Clinic. 5
Individuals with autoimmune-induced seizures typically do not respond to traditional seizure medications and treatments, and are often classified as having drug resistant epilepsy. 5
Others agree. Autoimmune factors may play a role in the onset of seizures in adults with no history and who do not respond to standard medication. “Accumulating evidence supports the role of autoimmune-mediated factors in patients with AED [antiepileptic drug]-resistant seizures.” 6
Identifying whether an autoimmune condition is causing the seizures or drug resistant epilepsy is important since treatment with immunotherapies can dramatically impact chances of recovery. 7 In fact, one study found 81% of patients had “significant improvement in seizure status” and 67% achieved “seizure freedom, a majority of whom were antiepileptic drug [AED] resistant.” 7
Identifying whether an autoimmune condition is causing the seizures or drug resistant epilepsy is important since treatment with immunotherapies can dramatically impact chances of recovery. 7
One study found 81% of patients had “significant improvement in seizure status” and 67% achieved “seizure freedom, a majority of whom were antiepileptic drug [AED] resistant.” 7
Autoantibodies, encephalitis and seizures
A growing number of autoantibodies are being identified and linked with seizures that have no known cause. “Specific autoimmune causes, typically associated with autoantibodies, have been increasingly identified in a subset of previously idiopathic seizure disorders.” 8
Others report, “it is widely believed that antibodies targeting against intracellular antigens or neuronal surface antigens are the potential causes [of idiopathic seizures].” 6
Several studies report the presence of specific neural autoantibodies in patients with autoimmune epilepsy, including antibodies against the NMDA receptor, AMPA receptors, LGI1 protein, and GABAb receptor.
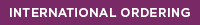
In some cases, autoimmune seizures may be the result of an infection-triggered autoimmune encephalopathy/encephalitis. This occurs when the immune system produces antibodies meant to destroy a foreign substance (i.e. bacteria, virus) but instead mistakenly attack healthy tissue in the brain (autoantibodies), causing inflammation (encephalitis) and the onset of seizures in children and adults with no history of epilepsy.
In some cases, seizures may be due to an infection-triggered autoimmune encephalitis.
This occurs when the immune system produces antibodies meant to destroy a foreign substance (i.e. bacteria, virus) but instead mistakenly attack healthy tissue in the brain (autoantibodies), causing inflammation (encephalitis) and the onset of seizures in children and adults with no history of epilepsy.
How can infections trigger an autoimmune reaction and the onset of seizures?
“Certain infections are known to trigger encephalitis (brain inflammation) and epilepsy in children,” states Korff and Dale. 10
“Some of them directly infect the brain and cause a primary viral encephalitis; on the other hand, certain micro-organisms can induce a secondary autoimmune encephalitis.” For instance, herpes simplex and mycoplasma have the highest potential to result in ongoing epilepsy. 10
Cunningham Panel™ identifies autoimmune seizures
Researchers describe the case of a 15-year-old girl, who developed a sudden onset of neuropsychiatric symptoms along with “seizure-like” episodes. The patient’s anti-NMDAR antibody test was negative and MRI’s were normal. However, her Cunningham Panel™ test results were positive, which indicated that her symptoms, including the seizures, were likely caused by an autoimmune reaction, triggered by an infection(s).
The girl was treated with immunotherapy, including plasma exchange. After 2 weeks of treatment, her symptoms had completely resolved. 11
- Stephen, L.J., Brodie, M.J. Pharmacotherapy of Epilepsy. CNS Drugs 25, 89–107 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21254787
- Dubey D, Alqallaf A, Hays R, et al. Neurological autoantibody prevalence in epilepsy of unknown etiology. JAMA Neurol. 2017 https://jamanetwork.com/journals/jamaneurology/fullarticle/2599939
- Ong M, Kohane IS, Cai T, Gorman MP, Mandl KD. Population-Level Evidence for an Autoimmune Etiology of Epilepsy. JAMA Neurol. 2014;71(5):569–574. doi:10.1001/jamaneurol.2014.188 https://jamanetwork.com/journals/jamaneurology/fullarticle/1851479
- Amanat, Man et al. Seizures as a clinical manifestation in somatic autoimmune disorders. Seizure - European Journal of Epilepsy, Volume 64, 59 - 64 https://www.seizure-journal.com/article/S1059-1311(18)30589-2/fulltext
- MedPage Today. Nyberg. Identification and Treatment of Autoimmune Epilepsy. July 13, 2018. https://www.medpagetoday.com/resource-centers/contemporary-advances-epilepsy/identification-and-treatment-autoimmune-epilepsy/2088
- Fang Z, Yang Y, Chen X, et al. Advances in Autoimmune Epilepsy Associated with Antibodies, Their Potential Pathogenic Molecular Mechanisms, and Current Recommended Immunotherapies. Front Immunol. 2017;8:395. Published 2017 Apr 25. doi:10.3389/fimmu.2017.00395 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5403900/
- Quek AM, Britton JW, McKeon A, et al. Autoimmune epilepsy: clinical characteristics and response to immunotherapy. Arch Neurol. 2012;69(5):582–593. doi:10.1001/archneurol.2011.2985 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601373/
- Ong MS, Kohane IS, Cai T, Gorman MP, Mandl KD. Population-level evidence for an autoimmune etiology of epilepsy. JAMA Neurol. 2014;71(5):569–574. doi:10.1001/jamaneurol.2014.188 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4324719/
- Dubey, Divyanshu et al. Retrospective case series of the clinical features, management and outcomes of patients with autoimmune epilepsy. Seizure - European Journal of Epilepsy, Volume 29, 143-147 https://www.ncbi.nlm.nih.gov/pubmed/26076858
- Christian M. Korff, Russell C. Dale. The Immune System in Pediatric Seizures and Epilepsies. Pediatrics Sep 2017, 140 (3) e20163534; DOI: 10.1542/peds.2016-3534 https://pediatrics.aappublications.org/content/140/3/e20163534
- Barzman DH, Jackson H, Singh U, Griffey M, Sorter M, Bernstein JA. An Atypical Presentation of Pediatric Acute Neuropsychiatric Syndrome Responding to Plasmapheresis Treatment. Case Rep Psychiatry. 2018;2018:8189067. Published 2018 Jun 28. doi:10.1155/2018/8189067 https://www.ncbi.nlm.nih.gov/pubmed/30050718
Mounting evidence indicates that abnormal autoimmune activity can elicit a sudden onset of seizures in adults.
Learn more about how infections can trigger neuropsychiatric symptoms

Cunningham Panel™ helps identify an autoimmune disorder in child initially diagnosed with schizophrenia
Researchers describe a complex case involving a 15-year-old girl, who abruptly developed multiple neurologic and psychiatric symptoms.
The association between streptococcus pyogenes and tics/OCD
In this book chapter, Dr. Madeleine Cunningham explains the association between Group A strep and the onset of tics and/or OCD and their clinical manifestations in children with the autoimmune neuropsychiatric disorder, PANDAS.
Childhood infections can increase risk of mental illness in kids
Nationwide study finds both mild and severe infections can increase risk of mental disorders in children and adolescents..