PANDAS: Diagnosis and Treatment
A study by Swedo et al. found, “Separation anxiety was the most common co-morbid symptom in both the NIMH and community samples [of PANDAS patients] (92% and 86%, respectively), followed closely by school issues (81% and 75%), and sleep problems (71% for both).” 2
It can be challenging to recognize PANDAS as many of the co-morbid symptoms overlap with other neuropsychiatric illnesses. As a result, children with PANDAS syndrome are often misdiagnosed with a primary psychiatric illness or behavioral disorder, such as OCD, ADHD, oppositional defiant disorder, Tourette’s syndrome, autism spectrum disorder (ASD), and bipolar disorder.
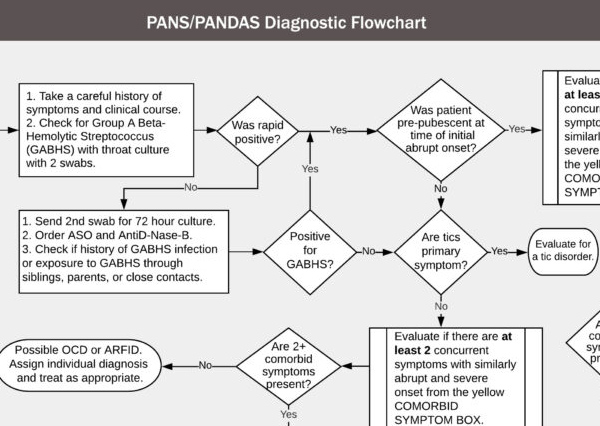
Diagnosing PANDAS can be challenging as symptoms follow a relapsing-remitting course and mimic many psychiatric disorders.
PANDAS is a clinical diagnosis made by a medical professional. The Cunningham Panel™ of tests can provide laboratory evidence of an underlying autoimmune dysfunction, and assist clinicians in their diagnosis and in determining an appropriate treatment regimen.
LEARN ABOUT TESTING
PANDAS: Diagnostic Criteria
- Presence of OCD and/or tics (particularly multiple, complex, or unusual tics)
- Symptoms of the disorder first become evident between 3 years of age and puberty
“Post-pubertal onset of PANDAS is possible and seen by NIMH and clinicians in the field.” 1
- Acute onset and episodic (relapsing-remitting) course
To meet the diagnostic criteria, symptoms must appear suddenly, seemingly overnight. However, there have been cases reported where symptom onset is more gradual.
- Association with Group A Streptococcal (GAS) infection
In PANDAS syndrome, “GAS infections often are found without apparent pharyngitis (i.e., the child did not complain of a sore throat).” 1
“40% of children with documented GAS infections do not show a titer rise, creating a potential false negative.” 1
- Association with Neurological Abnormalities
“The diagnostic criteria for PANDAS require only the presence of OCD or tics, but co-morbid neuropsychiatric symptoms are universally present.” 1
“… it is not uncommon for the type of co-morbid symptoms to change multiple times during the course of the illness.” 1
PANDAS: Treatment Guidelines
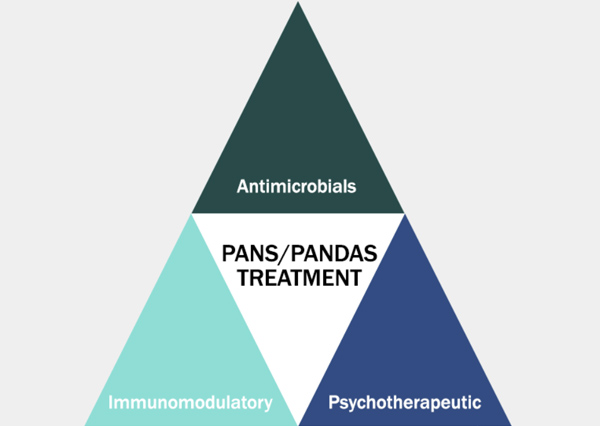
In 2017, a consortium of clinicians and researchers published PANS and PANDAS treatment guidelines in the Journal of Child and Adolescent Psychopharmacology. 3,4,5 The guidelines focused on three treatment areas: psychiatric and behavioral interventions, use of immunomodulatory therapies, and treatment and prevention of infections.
Although patients present with multiple neuropsychiatric symptoms, PANDAS is an autoimmune disorder, which may appear to be a primary psychiatric illness. The neuropsychiatric presentation can be confusing to parents and clinicians which may result in a missed or delayed diagnosis.
While psychotropic medications may be helpful in managing symptoms, often times patients with PANS and PANDAS do not respond to, or their symptoms are worsened with these medications.
Prompt treatment of each flare and treatment of the earliest flares improve outcomes. If flares are left untreated, the risks of ongoing neuropsychiatric symptoms and chronic inflammatory conditions are likely to increase. 6
It is important to identify and diagnose PANDAS early, as proper treatment can lead to a remarkable resolution or substantial reduction in symptoms.
PANDAS treatment involves identifying and eradicating any infections and addressing the underlying autoimmune dysfunction and inflammatory response with immunomodulatory therapies. Treatments may include antibiotics, steroids, anti-inflammatory drugs (such as ibuprofen or naproxen), CBT/ERP, psychotropics, intravenous immunoglobulin (IVIG), and plasmapheresis. 7
“Most patients with PANS/PANDAS remit with appropriate treatment. For a few children, the clinical course may evolve to become a chronic autoimmune condition.” 7
- PANDAS Physicians Network (PPN). PANDAS Diagnostic Guidelines. https://www.pandasppn.org/pandas/
- Swedo SE, Seidlitz J, Kovacevic M, et al. Clinical presentation of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections in research and community settings. J Child Adolesc Psychopharmacol. 2015;25(1):26-30. doi:10.1089/cap.2014.0073 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4340334/
- Margo Thienemann, Tanya Murphy, James Leckman, Richard Shaw, Kyle Williams, Cynthia Kapphahn, Jennifer Frankovich, Daniel Geller, Gail Bernstein, Kiki Chang, Josephine Elia, and Susan Swedo. Journal of Child and Adolescent Psychopharmacology.Sep 2017.566-573.http://doi.org/10.1089/cap.2016.0145 https://www.liebertpub.com/doi/full/10.1089/cap.2016.0145
- Jennifer Frankovich, Susan Swedo, Tanya Murphy, Russell C. Dale, Dritan Agalliu, Kyle Williams, Michael Daines, Mady Hornig, Harry Chugani, Terence Sanger, Eyal Muscal, Mark Pasternack, Michael Cooperstock, Hayley Gans, Yujuan Zhang, Madeleine Cunningham, Gail Bernstein, Reuven Bromberg, Theresa Willett, Kayla Brown, Bahare Farhadian, Kiki Chang, Daniel Geller, Joseph Hernandez, Janell Sherr, Richard Shaw, Elizabeth Latimer, James Leckman, Margo Thienemann, and PANS/PANDAS Consortium.Journal of Child and Adolescent Psychopharmacology.Sep 2017.574-593.http://doi.org/10.1089/cap.2016.0148 https://www.liebertpub.com/doi/full/10.1089/cap.2016.0148
- Michael S. Cooperstock, Susan E. Swedo, Mark S. Pasternack, Tanya K. Murphy, and for the PANS/PANDAS Consortium.Journal of Child and Adolescent Psychopharmacology.Sep 2017.594-606.http://doi.org/10.1089/cap.2016.0151 https://www.liebertpub.com/doi/full/10.1089/cap.2016.0151
- Margo Thienemann, MD, Jennifer Frankovich, MD, MS. Sudden Onset of Tics, Tantrums, Hyperactivity, and Emotional Lability: Update on PANS and PANDAS. Psychiatric Times. April 25, 2017. https://www.psychiatrictimes.com/view/sudden-onset-tics-tantrums-hyperactivity-and-emotional-lability-update-pans-and-pandas
- PANDAS Physicians Network (PPN). Treating PANS/PANDAS. https://www.pandasppn.org/treatment/

PANDAS patients often have multiple neuropsychiatric symptoms that may change over the course of illness.
Learn More About PANS & Pandas and The Cunningham Panel™
PANDAS Diagnostic Guidelines
PANDAS Treatment Guidelines