COVID-related syndrome MIS-C linked with cardiac complications in children
Multisystem inflammatory syndrome: diagnosis and treatment 2
A growing number of studies report that a subset of children and adolescents with COVID-19 may go on to develop a potentially life-threatening inflammatory condition known as Multisystem Inflammatory Syndrome in Children (MIS-C), in which one or more organs, including the heart, become severely inflamed.
As of February 1, 2021, the Centers for Disease Control and Prevention (CDC) reported over 2,600 cases of MIS-C in the U.S. and at least 33 deaths. 1
There are many unanswered questions about why some children and adolescents develop MIS-C after a COVID-19 illness, or contact with someone with COVID-19, while others do not.
MIS-C: a post-infectious myocarditis
In their review article, McMurray et al. discuss MIS-C as a post-infectious myocarditis and systemic vasculitis affecting the coronary arteries. 2 The authors describe the clinical presentation, immunopathogenesis, diagnosis and treatment of Multisystem Inflammatory Syndrome in Children (MIS-C) with a history of COVID-19 and compare it with other pediatric rheumatologic conditions affecting the heart, including Kawasaki disease (KD).
In the initial days of the COVID-19 pandemic, pediatric patients were typically asymptomatic or presented with mild disease. In April 2020, a more complex post-viral condition emerged as children “began presenting with fever, gastrointestinal symptoms and features of myocarditis, including some with coronary artery aneurysms (CAAs), as clusters in the Western hemisphere,” the authors report.
Most of these children had negative COVID-19 testing by nasopharyngeal reverse-transcriptase polymerase chain reaction (RT-PCR), but positive serum levels of anti-SARS-CoV2 antibodies, which suggested that MIS-C was a post-viral inflammatory disease rather than an unremitting infection.
The clinical presentation of MIS-C shares many similarities with Kawasaki disease (KD), and most notably, for causing CAA [coronary artery aneurisms] in almost 1 in 5 patients.
It has been observed that KD and MIS-C share two major commonalities impacting the innate immune system, that being endothelial cell activation and the upregulation of the IL-1β pathway. Upon activation of IL-1β there is a downstream increase in the expression of many proinflammatory cytokines.
Treatment focuses on anti-inflammatory therapies
Therefore, clinical management has focused on certain anti-inflammatory modalities to reduce tissue inflammation and limit the progression of coronary artery aneurisms (CAA) and cardiac injury.
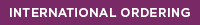
MIS-C has a broad range of clinical presentations, making diagnosis challenging. Yet, the authors urge, “prompt recognition and treatment is critical to minimize risk for cardiac decompensation and development of coronary artery aneurysms.”
As many aspects of multisystem inflammatory syndrome in children (MIS-C) remain undiscovered, there is need for collective and global efforts to fast-tracked patient-centered research.
- SARS-CoV-2 has the potential to cause post-infectious myocarditis, and the underlying pathogenesis is expected to be similar across all ages.
- The clinical presentation of MIS-C shares many similarities with Kawasaki disease (KD), and most notably, for causing CAA [coronary artery aneurisms] in almost 1 in 5 patients. The clinical course, however, varies widely compared with KD.
- Treatment of MIS-C includes antibiotics, IVIG and aspirin, with corticosteroids, and biological response modifier drugs, such as Anakinra, prescribed for more severe cases. “In concurrent use with IVIG, steroids have resulted in rapid recovery in those patients presenting with severe features of MIS-C.”
- Anti-inflammatory treatment is aimed to reduce tissue inflammation to prevent or limit the progression of coronary artery aneurisms and cardiac injury. “In MIS-C patients treated with IVIG, rapid resolution of symptoms has been commonly reported.”
HIGH PREVALENCE OF NEUROPSYCHIATRIC COMPLICATIONS OF COVID-19 3
Largest review to date examines effects of Coronavirus
This is believed to be the largest and most comprehensive systematic review to date of neurological and neuropsychiatric manifestations of COVID-19 with a total population of 105,638 patients worldwide included in the study. 3 (Note: This article has not been peer-reviewed.)
Neurological and neuropsychiatric comorbidity is likely to be the norm rather than the exception in COVID-19.
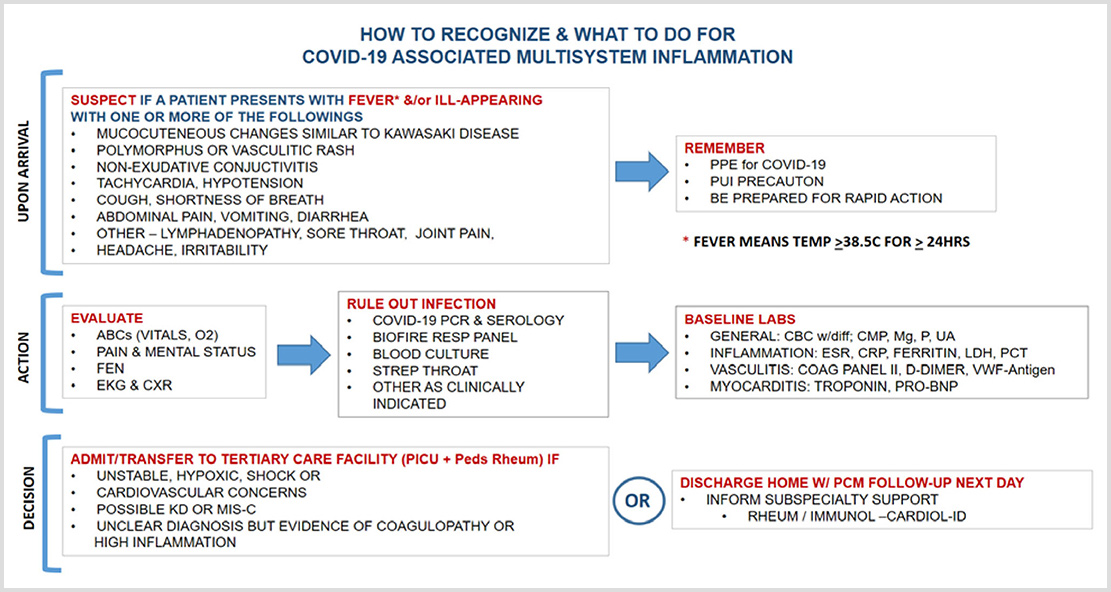
According to the authors, neurological and neuropsychiatric symptoms are very common with more than 30% of COVID-19 patients experiencing headache, myalgia, fatigue, anosmia and dysgeusia. These non-specific symptoms occur more frequently, followed by neuropsychiatric complications such as anxiety and depression, which have been reported in as many as 23% of patients.
Investigators warn, “given the multitude of symptoms reported, neurological and neuropsychiatric comorbidity is likely to be the norm rather than the exception in COVID-19, so there must be accessible advice and input from these specialties for patients who are acutely unwell.”
Schedule: In-services for utilization of the Cunningham Panel™
We provide free, medical education services to assist clinicians in better understanding the Cunningham Panel™ utilization of results. This service is open to individual clinicians and group practices.
Additional Studies
- Centers for Disease Control and Prevention. https://www.cdc.gov/mis-c/cases/
- McMurray JC, May JW, Cunningham MW, Jones OY. Multisystem Inflammatory Syndrome in Children (MIS-C), a Post-viral Myocarditis and Systemic Vasculitis-A Critical Review of Its Pathogenesis and Treatment. Front Pediatr. 2020 Dec 16;8:626182. doi: 10.3389/fped.2020.626182. PMID: 33425823; PMCID: PMC7793714.
- Rogers J. et al. The neurology and neuropsychiatry of COVID-19: a systematic review and meta-analysis of the early literature reveals frequent CNS manifestations and key emerging narratives. medRxiv, 2/26/2021. https://doi.org/10.1101/2021.02.24.21252335
Digital Information Packet
To learn more about infection-triggered basal ganglia encephalitis syndromes, such as PANS/PANDAS, view our online informational packet. We have compiled journal articles and video clips that may be helpful to you.