What is PANS?
PANS is a broader clinical diagnostic category which includes PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections). PANS and PANDAS are immune-mediated conditions that result in autoimmune encephalopathy (AE) or basal ganglia encephalitis (BGE). However, while PANDAS is a disorder that is preceded by a strep infection, PANS is a syndrome which may be triggered by other infections or even environmental triggers.
PANS: Neuropsychiatric Symptoms
PANS symptoms can vary from person to person, range in severity, but follows a relapsing/remitting course.
This syndrome is characterized by an abrupt onset of obsessive-compulsive behaviors or restrictive eating accompanied by other neuropsychiatric symptoms which may include anxiety, emotional lability, depression, irritability, aggression, oppositional behavior, deterioration in school performance, behavioral (developmental) regression, sensory amplification, movement abnormalities, sleep disturbance, and urinary frequency. 1
“PANS symptoms overlap with a variety of psychiatric disorders, such as OCD, Tourette’s syndrome, ADHD, depression, and bipolar disorder. However, the acuity of onset and simultaneous presentation of these symptoms differentiate PANS from these psychiatric conditions.” 1
A number of infections have been associated with the onset of PANS including upper respiratory infections, such as rhinosinusitis, pharyngitis, or bronchitis, mycoplasma pneumoniae, influenza, Epstein Barr virus, Borrelia burgdorferi (Lyme disease), herpes simplex infection and varicella. 2
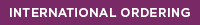
Researchers now recognize that infections and inflammation can open up the blood-brain barrier, permitting autoantibodies to enter the brain, resulting in neurologic and psychiatric symptoms. 3
In PANS and PANDAS, autoantibodies target components located in the basal ganglia region of the brain. These targets may include the Dopamine D1 receptor, Dopamine D2 receptor, Lysoganglioside GM1, and Tubulin. When antibodies bind to or block these targets they disrupt functioning, resulting in neuropsychiatric symptoms. 2
- Kiki Chang, Jennifer Frankovich, Michael Cooperstock, Madeleine W. Cunningham, M. Elizabeth Latimer, Tanya K. Murphy, Mark Pasternack, Margo Thienemann, Kyle Williams, Jolan Walter, Susan E. Swedo, and From the PANS Collaborative Consortium.Journal of Child and Adolescent Psychopharmacology.Feb 2015.3-13.http://doi.org/10.1089/cap.2014.0084 https://www.liebertpub.com/doi/full/10.1089/cap.2014.0084/li>
- Chain JL, Alvarez K, Mascaro-Blanco A, et al. Autoantibody Biomarkers for Basal Ganglia Encephalitis in Sydenham Chorea and Pediatric Autoimmune Neuropsychiatric Disorder Associated With Streptococcal Infections. Front Psychiatry. 2020;11:564. Published 2020 Jun 24. doi:10.3389/fpsyt.2020.00564 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7328706//li>
- Benros ME, Waltoft BL, Nordentoft M, et al. Autoimmune Diseases and Severe Infections as Risk Factors for Mood Disorders: A Nationwide Study. JAMA Psychiatry. 2013;70(8):812–820. doi:10.1001/jamapsychiatry.2013.1111 https://jamanetwork.com/journals/jamapsychiatry/fullarticle/1696348/li>
Learn More About PANS & Pandas and The Cunningham Panel™

PANS: Diagnosis and Treatment

Patient Stories