Compulsions
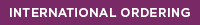
Infections and treatment resistant OCD
Patients with treatment resistant OCD can suffer terribly with little relief. “Some people suggest that the level of functioning in someone with treatment resistant OCD is about the level of functioning of a patient with schizophrenia.” 2
The outlook for children is just as sobering. Bloch et al. found that over 46% of children diagnosed with OCD did not achieve a remission. “Children with OCD symptoms that do not respond to evidence-based treatments are among the most challenging and difficult patients with OCD to treat.” 3
It is unknown why some patients with treatment resistant OCD don’t respond to standard medications. There may be multiple factors at play.
Autoimmune induced OCD
New research indicates that some patients with OCD, who do not respond to standard treatment or whose symptoms worsen with these medications, may have a form of autoimmune encephalitis, known as basal ganglia encephalitis, prompting their OCD-like behaviors.
Various infections, including strep, mycoplasma pneumonia and coxsackie virus, can trigger the immune system to produce antibodies that mistakenly target a specific region of the brain, leading to basal ganglia encephalitis.
For instance, strep infections can trigger neuropsychiatric symptoms, including obsessive compulsive behaviors, in a subset of children. An estimated 1 in 200 children in the U.S. are believed to suffer from PANDAS, pediatric autoimmune neuropsychiatric disorders associated with strep infections. 5
Additionally, Orlovska et al. found that “individuals with a streptococcal throat infection had elevated risks of mental disorders, particularly OCD and tic disorders.” 6
Other infectious agents have been linked with obsessive compulsive behaviors. People with toxoplasmosis had 2.5 times higher odds of developing OCD, according to one study. 7 And herpes simplex virus, mycoplasma pneumoniae, measles, chicken pox, cytomegalovirus, mumps 8 and Borrelia burgdorferi, the bacteria which causes Lyme disease 9 have all been associated with the onset of OCD-like symptoms.
- Flegr, J. et al. Toxoplasma-infected subjects report an Obsessive-Compulsive Disorder diagnosis more often and score higher in Obsessive-Compulsive Inventory. European Psychiatry. Volume 40, 82-87. https://www.ncbi.nlm.nih.gov/pubmed/27992837
- Hollander, E. Interview: Developing Guidelines for Treatment-Resistant OCD. Medscape. https://www.medscape.org/viewarticle/507104
- Bloch MH, Storch EA. Assessment and management of treatment-refractory obsessive-compulsive disorder in children. J Am Acad Child Adolesc Psychiatry. 2015;54(4):251–262. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4460245
- Attwells S, Setiawan E, Wilson AA, et al. Inflammation in the Neurocircuitry of Obsessive-Compulsive Disorder. JAMA Psychiatry. 2017;74(8):833–840. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2631893
- PANDAS Network, Statistics. http://pandasnetwork.org/statistics/
- Orlovska S, Vestergaard CH, Bech BH, Nordentoft M, Vestergaard M, Benros ME. Association of Streptococcal Throat Infection With Mental Disorders: Testing Key Aspects of the PANDAS Hypothesis in a Nationwide Study [published online May 24, 2017]. JAMA Psychiatry. 2017; doi: 10.1001/jamapsychiatry.2017.0995. https://jamanetwork.com/journals/jamapsychiatry/article-abstract/2629065
- Lamothe H, Baleyte JM, Smith P, Pelissolo A, Mallet L. Individualized Immunological Data for Precise Classification of OCD Patients. Brain Sci. 2018;8(8):149. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6119917
- Khanna S, Ravi V, Shenoy PK, Chandramukhi A, Channabasavanna SM. Viral antibodies in blood in obsessive compulsive disorder. Indian J Psychiatry. 1997;39(3):190–195. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2967113
- Carly Johnco, Brittany B. Kugler, Tanya K. Murphy, Eric A. Storch, Obsessive-compulsive symptoms in adults with Lyme disease. General Hospital Psychiatry. Volume 51, 2018, Pages 85-89. https://www.ncbi.nlm.nih.gov/pubmed/29408088
Learn more about how infections can trigger neuropsychiatric symptoms

Cunningham Panel™ helps identify an autoimmune disorder in child initially diagnosed with schizophrenia
Researchers describe a complex case involving a 15-year-old girl, who abruptly developed multiple neurologic and psychiatric symptoms.
The association between streptococcus pyogenes and tics/OCD
In this book chapter, Dr. Madeleine Cunningham explains the association between Group A strep and the onset of tics and/or OCD and their clinical manifestations in children with the autoimmune neuropsychiatric disorder, PANDAS.
Childhood infections can increase risk of mental illness in kids
Nationwide study finds both mild and severe infections can increase risk of mental disorders in children and adolescents..